All About
Breast Reconstruction
For more information on support groups, financial incentives, and additional resources, please visit our Breast Cancer Resource Center page.
Breast Cancer Resource Center
Procedure Video
Reconstruction After Mastectomy
A mastectomy is a surgical procedure to remove all or most of the breast tissue, typically performed as part of breast cancer treatment or to reduce the risk of breast cancer in high-risk individuals.
There are different types of mastectomies, including:
Simple (Total) Mastectomy: Removal of the entire breast, including the nipple and areola.
Skin-Sparing Mastectomy: Breast tissue is removed, but most of the natural breast skin is preserved for reconstruction.
Nipple-Sparing Mastectomy: The breast tissue is removed while preserving the natural skin, nipple, and areola.
Many women choose to undergo breast reconstruction after mastectomy to help restore the breast’s shape and appearance, either at the same time (immediate reconstruction) or at a later date (delayed reconstruction).
What is a Mastectomy?
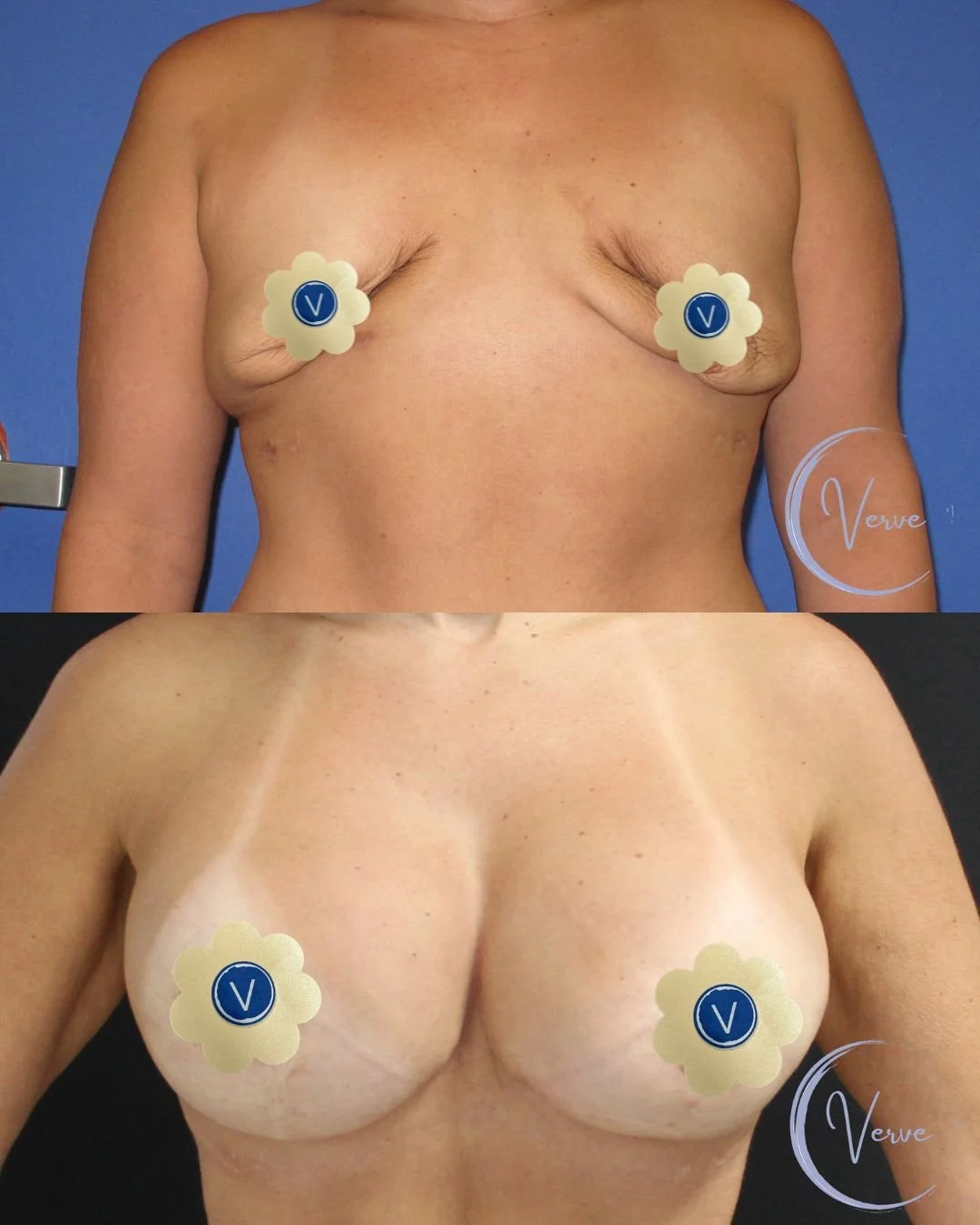
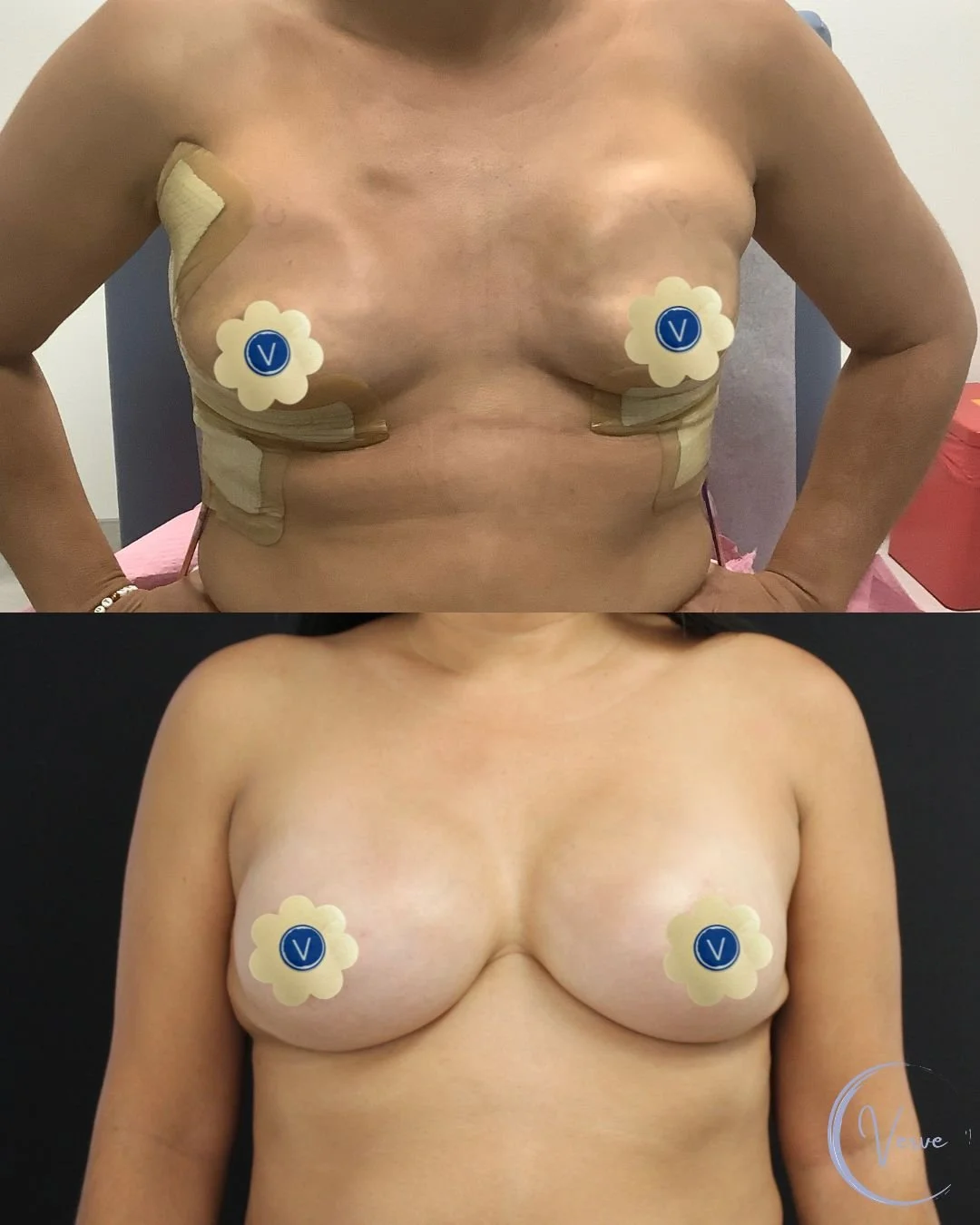
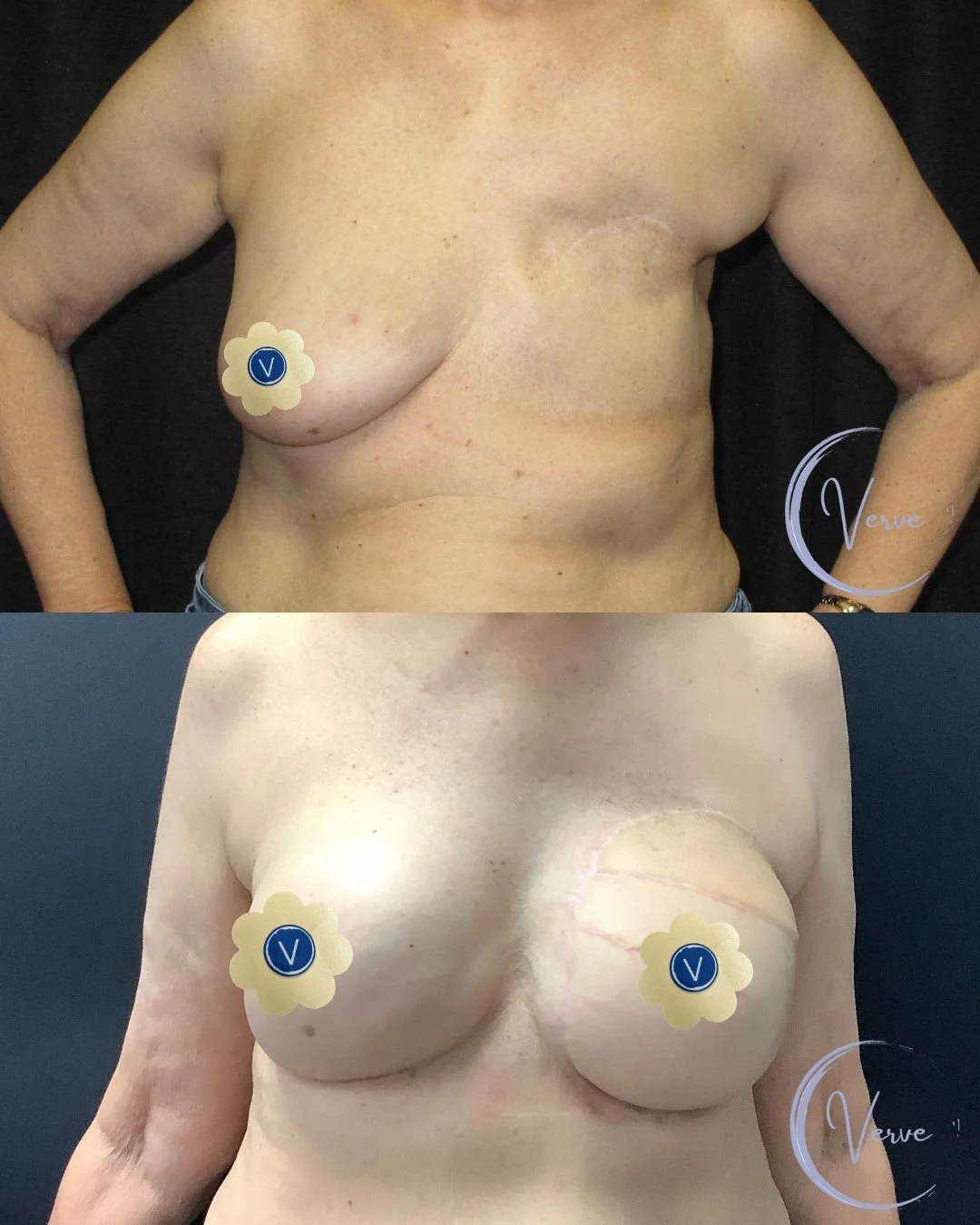
Reconstruction Phases Post Mastectomy
-
The first step in reconstruction begins with the mastectomy, a procedure performed by your general surgeon to remove breast tissue affected by cancer or as a preventive measure. This creates the foundation for reconstruction and can be done on one or both breasts, depending on your treatment plan.
-
Immediately following the mastectomy, Dr. Gupta will place a tissue expander beneath the chest muscle. This temporary device acts like a balloon, gradually stretching the skin and muscle over time to make room for a permanent implant. It’s a crucial first step in rebuilding the breast shape and setting the stage for a natural-looking result.
-
Over the next few weeks or months, you’ll come in for expansion appointments, where Dr. Gupta will slowly fill the expander with saline to gently stretch the tissue. This process is typically well-tolerated and allows your body to adjust gradually. Once the desired size is reached and the skin has healed, you’ll be ready for Phase 2.
Phase 1: Mastectomy + Tissue Expander
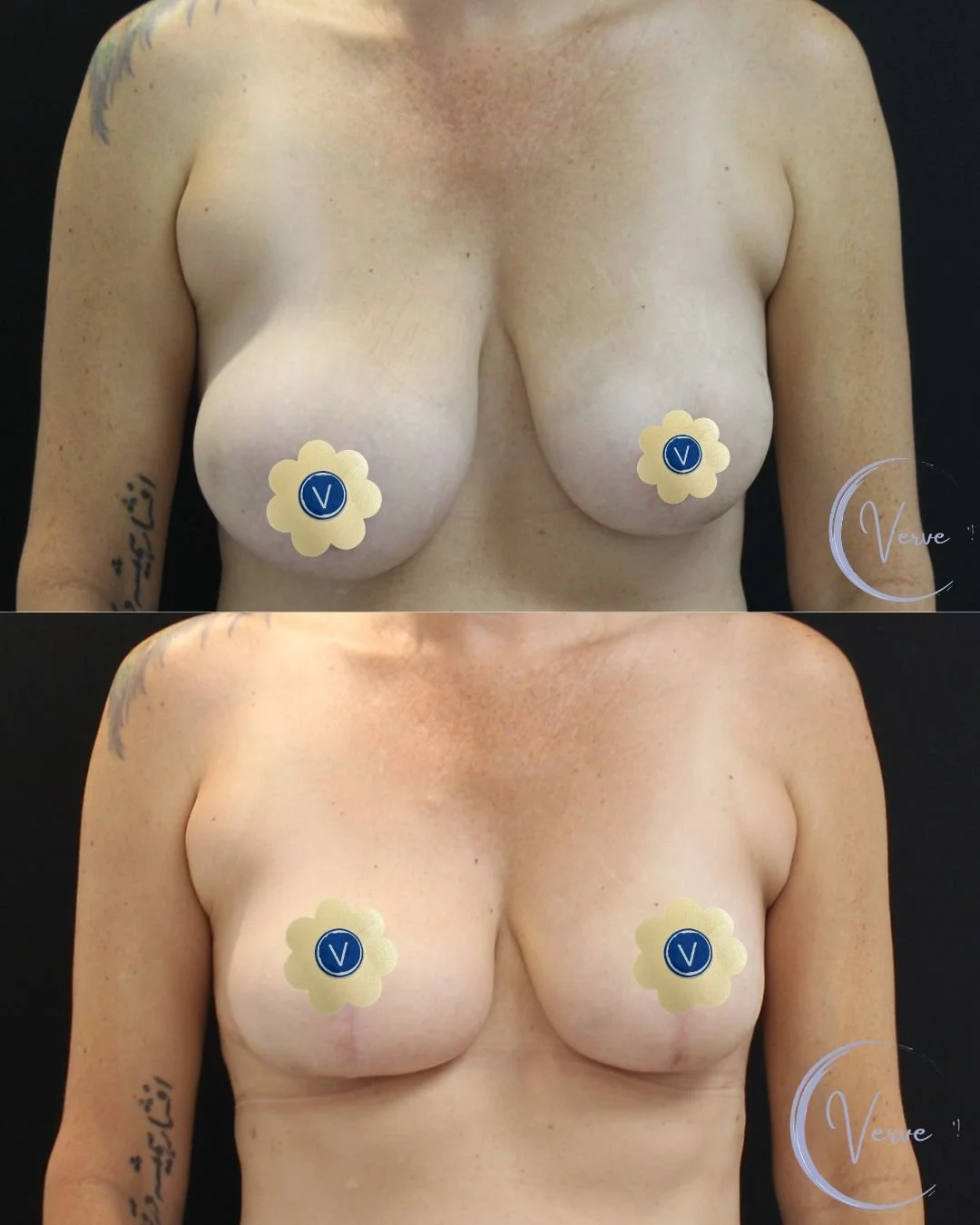
Phase 2: Tissue Expander to Breast Implant Exchange
-
Once your tissue expansion is complete and the skin and muscle have had time to heal, you’ll move on to Phase 2: exchanging the tissue expander for a permanent breast implant. This typically takes place a few months after your mastectomy and expansion process, depending on your healing and any additional treatments like chemotherapy or radiation.
-
Dr. Gupta will remove the tissue expander and replace it with a soft, natural-feeling breast implant—either silicone or saline, depending on your preference and anatomy. This procedure is generally less invasive than the initial surgery and often involves a shorter recovery time. The goal is to create a breast shape that looks and feels more natural.
-
Recovery from implant exchange is typically quicker and more comfortable than Phase 1. Most patients return to light activity within a few days. After surgery, your breasts will look more defined and natural compared to when the tissue expanders were in place, though they may still feel slightly firm or misshaped at first. This is completely normal. The final shaping and refinement of your breast reconstruction usually takes place during Phase 3, which may include fat grafting or nipple reconstruction.
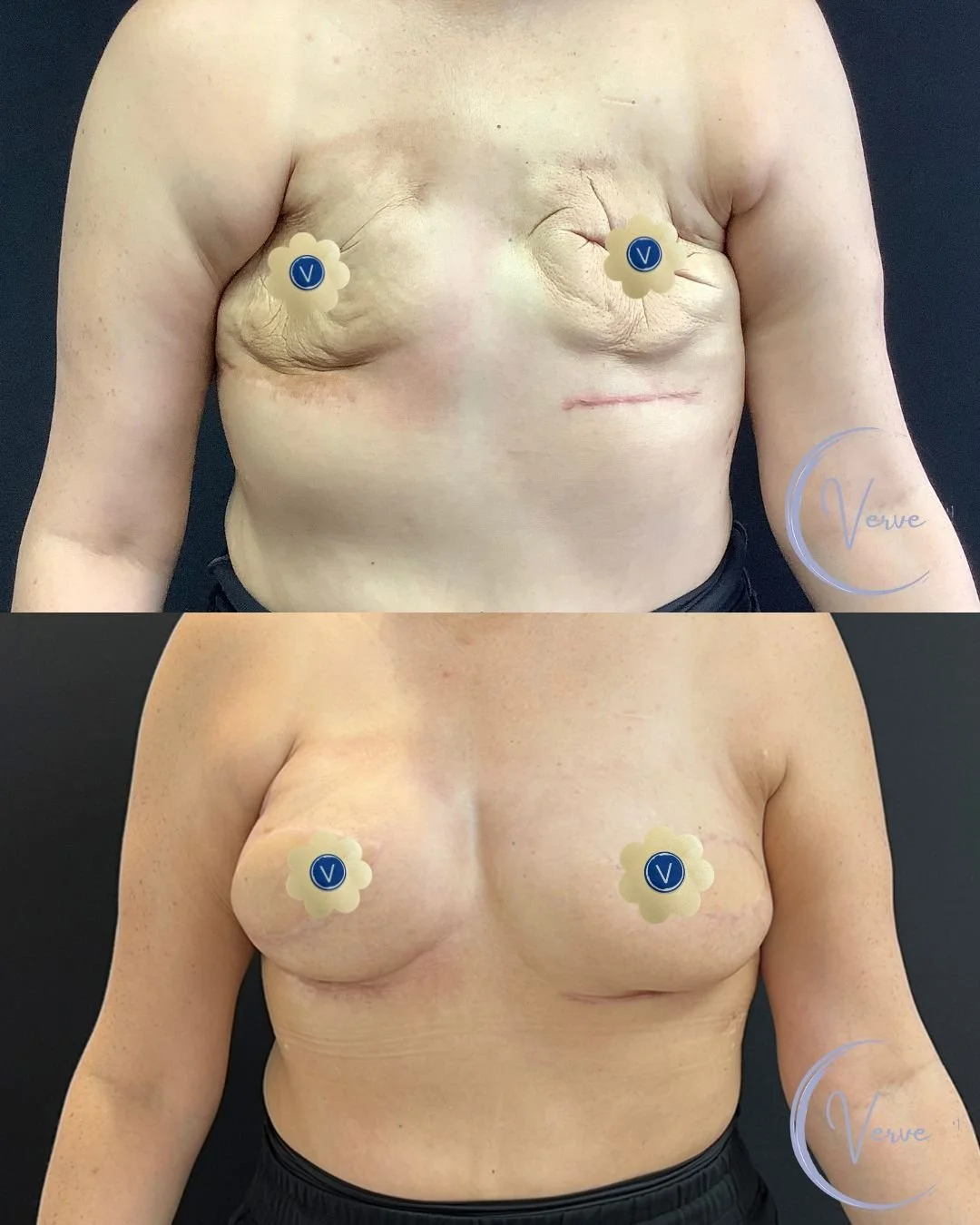
Phase 3: Fat Grafting, Nipple Reconstruction, Paramedical Nipple and Areola Tattooing
-
Phase 3 focuses on refining the look and feel of your reconstructed breasts. Fat grafting is often used to add softness, correct contour irregularities, and enhance symmetry. Fat is gently liposuctioned from another area of your body—like the abdomen or thighs—and carefully injected into the breast to smooth out any hollowness or unevenness left from earlier stages.
-
Some mastectomy patients retain their natural nipples, while others may lose them during surgery, depending on the type of mastectomy performed. If you’ve lost your nipples, you have the option to undergo nipple reconstruction, where Dr. Gupta uses a small flap of your own skin to recreate a natural-looking nipple. This minor procedure is typically done under local anesthesia and helps restore a more complete, natural breast appearance.
-
Once the nipple area has healed, paramedical tattooing can be done to add realistic color and dimension to the areola. Whether or not you’ve had nipple reconstruction, tattooing provides the final visual detail, bringing a natural-looking finish to your reconstruction journey.
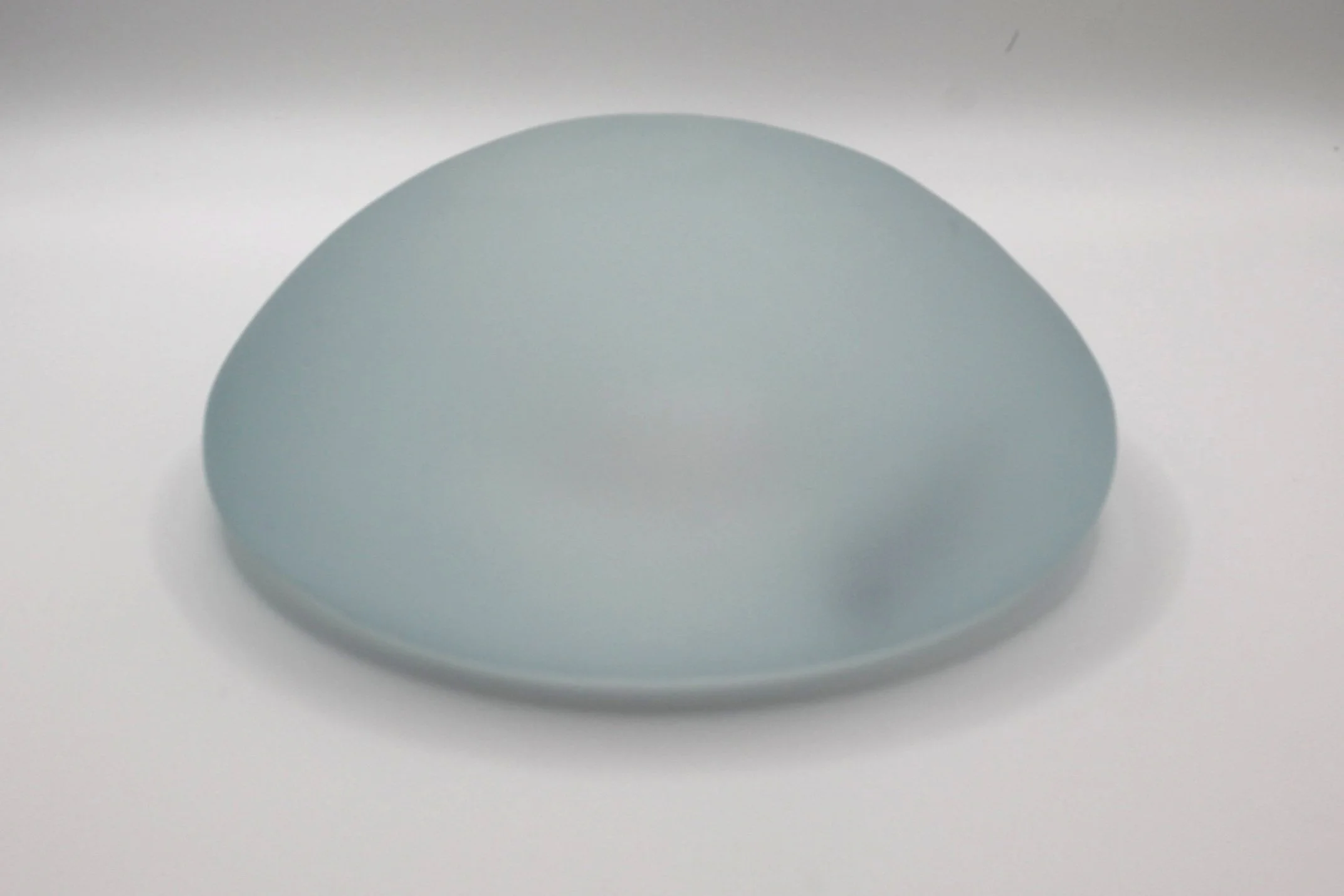
Tissue Expander
-
A tissue expander is a temporary implant used to gradually stretch the skin and muscle after a mastectomy to prepare for permanent breast reconstruction. It acts as a placeholder that creates space for a future breast implant or flap reconstruction.
-
After the tissue expander is placed, small amounts of saline are gradually injected into the expander over several weeks or months. This gently stretches the skin and soft tissue to accommodate the final breast implant.
-
Most patients experience mild pressure or tightness after each expansion, but discomfort is usually short-lived and manageable with over-the-counter medication.
-
The expander typically stays in place for a few months, depending on how much expansion is needed and your healing process. Once the desired size is achieved, Dr. Gupta will perform a second surgery to remove the expander and place the permanent implant or perform your chosen reconstruction.
-
Yes! One of the benefits of using a tissue expander is that it allows you and Dr. Gupta to adjust and personalize the breast size gradually, giving you time to decide what feels right for you.
-
While you have the tissue expander in place, your breasts may look temporary, firmer, and less natural in shape compared to the final result. The expander creates a rounded, sometimes higher appearance as the skin and tissue gradually stretch. This is a normal part of the process, and once the expander is removed and the final implant or reconstruction is completed, your breasts will have a softer, more natural contour.
Paramedical Nipple and Areola Tattooing
-
It's a specialized tattooing technique that recreates the look of a natural nipple and areola using custom-blended pigments, often performed after breast reconstruction.
-
Yes. 3D shading and color matching create a highly realistic, natural-looking result—even giving the illusion of texture and depth.
-
Most patients report little to no discomfort. The area often has reduced sensitivity due to surgery, and a numbing cream can be applied if needed.
-
The tattoo typically lasts several years. A touch-up may be needed over time as pigments naturally fade.
-
You should wait until the area is fully healed—usually 3 to 6 months after breast reconstruction.
View the Gallery
Hear Stories From Our Breast Reconstruction Patients
-
[Title screen for Lynn’s Story – Breast Reconstruction]
[Lynn, the Breast Reconstruction Patient, speaking to the camera like an interview]
I only had a mastectomy on one side and that was the side that sort of started shrinking and because I had fat put into that side to recreate a breast and that fat started like breaking down over the years because I had the breast cancer 15 years ago and I did not even realize that it was possible to fix that and then over the years it got worse and worse and worse to the point where my right side was a B cup, the left side was a double D and it really bothered me and so I was so relieved to know that it could be fixed.
[Patient sitting with Dr. Gupta in a consultation appointment]
I cannot speak highly enough about Dr. Gupta and how comfortable he made me feel because he’s very warm and he makes you feel welcome and he takes his time to talk to you in a gentle way.
[Lynn, the Breast Reconstruction Patient, speaking to the camera like an interview]
And when I first came here with my breast cancer situation, you know it was emotional for me and I was even crying in his office and everything and he just made it feel, it made me feel like it’s all okay.
[Closing title screen with Verve Plastic Surgery logo]
[On-screen text: Call today (760) 436-7600]
-
[Title screen for Cynthia’s Story – Breast Reconstruction]
[Cynthia, breast reconstruction patient, talking to the camera like an interview]
Well my husband found a lump in my breast. At first we didn’t know how advanced it was. The results came back that it wasn’t good and I would have to remove one or both breasts. I was really devastated because I was told 40 percent chance to keep one breast, 20 to keep the other. The outlook did not seem good. I decided to go ahead with the double mastectomy for both breasts. I thought that was best at the time for myself and for my family.
[Dr. Gupta in the operating room performing the breast reconstruction procedure]
Dr. Gupta did the reconstruction with Alison. I can’t even put into words how comforting they made me and how easy it ended up being. He was calmly confident
[Cynthia, breast reconstruction patient, talking to the camera like an interview]
and that really helped me a lot.
[Cynthia in a consultation appointment with Dr. Gupta]
He listened to all my concerns. He listened to my tears and his team were so calm with me and understanding but so confident that my breast after reconstruction would be twins as he called it. They would be perfect. And they are.
[Cynthia, breast reconstruction patient, talking to the camera like an interview]
He is the best. I mean, I did my own research out of every plastic surgeon in this area up to LA, and he was my first pick. My breast surgeon also had recommended him highly, so I was two for two, and I’m very happy with the choice that I made.
[Cynthia in a consultation appointment with Dr. Gupta]
How he did that, considering what they looked like after my double mastectomy,
[Cynthia, breast reconstruction patient, talking to the camera like an interview]
he’s a genius because I still don’t believe it.
[Cynthia in a consultation appointment with Dr. Gupta]
So I’m extremely happy. I’m very thankful for the whole team here. They’ve given me my life back and
[Cynthia, breast reconstruction patient, talking to the camera like an interview]
I always said to them if I could be of help to any other cancer patient knowing what I know now, I would love to.
[Closing title screen with Verve Plastic Surgery logo]
[On-screen text: Call today (760) 436-7600]
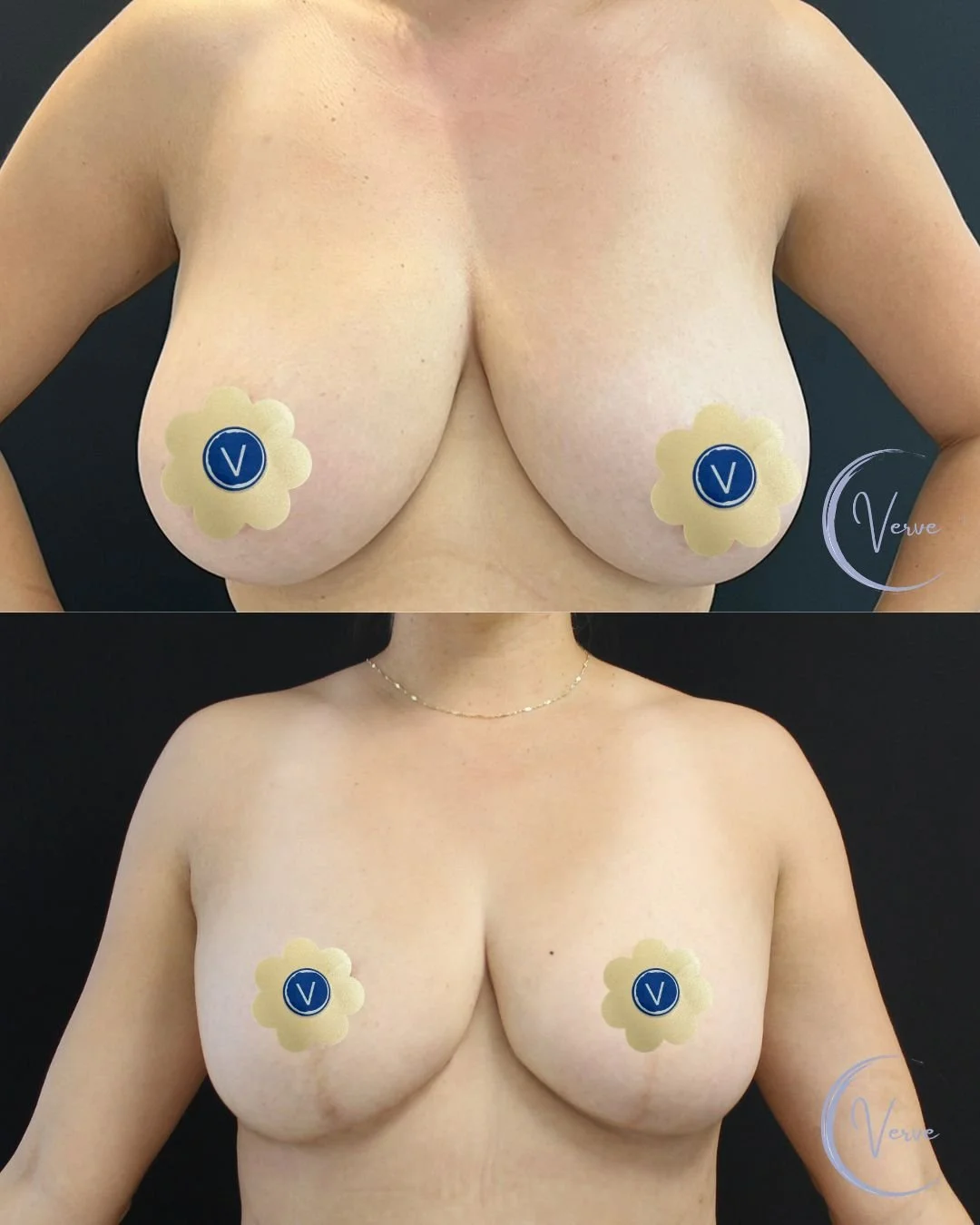
Reconstruction After Lumpectomy
What is a Lumpectomy?
A lumpectomy is a surgical procedure to remove breast cancer or abnormal tissue along with a small amount of surrounding healthy tissue. Unlike a mastectomy, which removes the entire breast, a lumpectomy is considered a breast-conserving surgery because it aims to preserve as much of the natural breast as possible.
Lumpectomy is often followed by radiation therapy to reduce the risk of cancer returning. Some women choose to have breast reconstruction after a lumpectomy—especially if the surgery leaves noticeable differences in breast size, shape, or symmetry.
Hear From Our Breast Reconstruction Patient
-
[Title screen for Tiffany’s Story – Breast Reconstruction]
[Tiffany, breast reconstruction patient, talking to the camera like an interview]
So getting a diagnosis of breast cancer is very overwhelming. You come to feel like your life is spinning out of control and you’re trying your best to regain that control with every decision that you’re faced with. So personally I researched everything. So I work in the surgical environment and have for many years and I always suggest that when you’re faced with having a surgical procedure of any kind, it’s a good idea to get the opinions of the surgical nurses on what doctor they recommend. And so I was able to talk to the nurses that I work with and one in particular said to me that she was so glad to hear that I was teamed up with Dr. Gupta because she said if I was able to recommend anybody to you, he would be my first choice and after meeting him
[Tiffany in a consultation appointment with Dr. Gupta]
I realized she was right. I was fortunate to be paired with the best of the best. My first appointment was amazing. They really walk you through this process and they handle it in a way that makes you so comfortable. He spent time with me. I wasn’t really expecting that either. A lot of these appointments can feel rushed, but he gave me all of his attention and all of his time and
[Tiffany, breast reconstruction patient, talking to the camera like an interview]
I felt like I was able to ask everything that was on my mind and
[Tiffany admiring her body post procedure in the mirror]
I have to say today things are great. I was very pleased with the reconstruction.
[Tiffany, breast reconstruction patient, talking to the camera like an interview]
I’ve seen pictures of other people’s work and I know I chose the right person for the job.
[Tiffany in a consultation appointment with Dr. Gupta]
I definitely feel like I have more confidence. He made me look better than I did before with my own natural breast.
[Tiffany, breast reconstruction patient, talking to the camera like an interview]
And I had had an oncology surgeon tell me to manage my expectations with breast reconstruction, that it’s not the same thing as breast augmentation, but honestly with Dr. Gupta’s work, you almost can’t tell the difference between augmentation and the reconstruction, it’s that good of a job.
[Closing title screen with Verve Plastic Surgery logo]
[On-screen text: Call today (760) 436-7600]
[Closing title screen with Verve Plastic Surgery logo]
[On-screen text: Call today (760) 436-7600]
View the Gallery
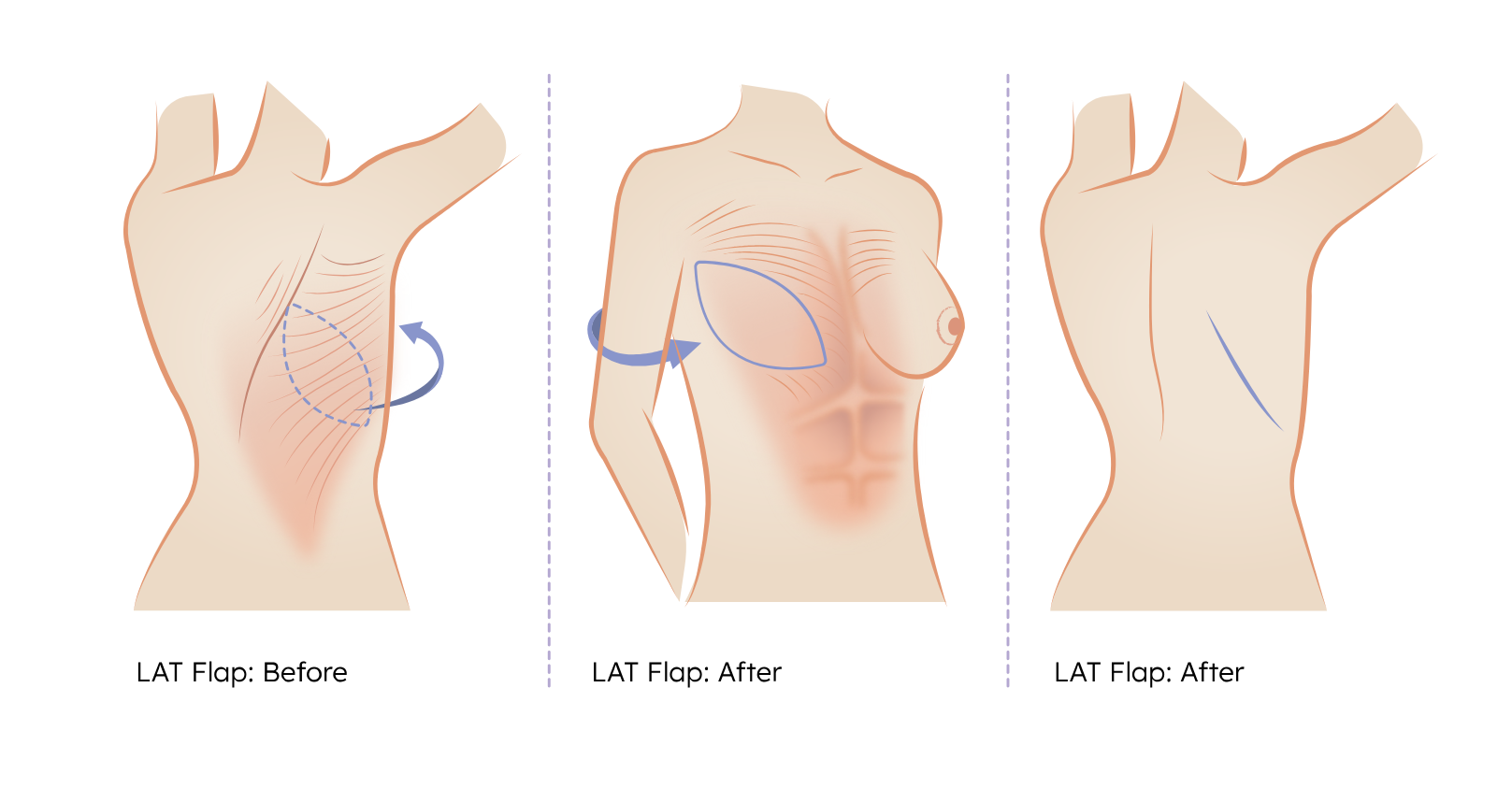
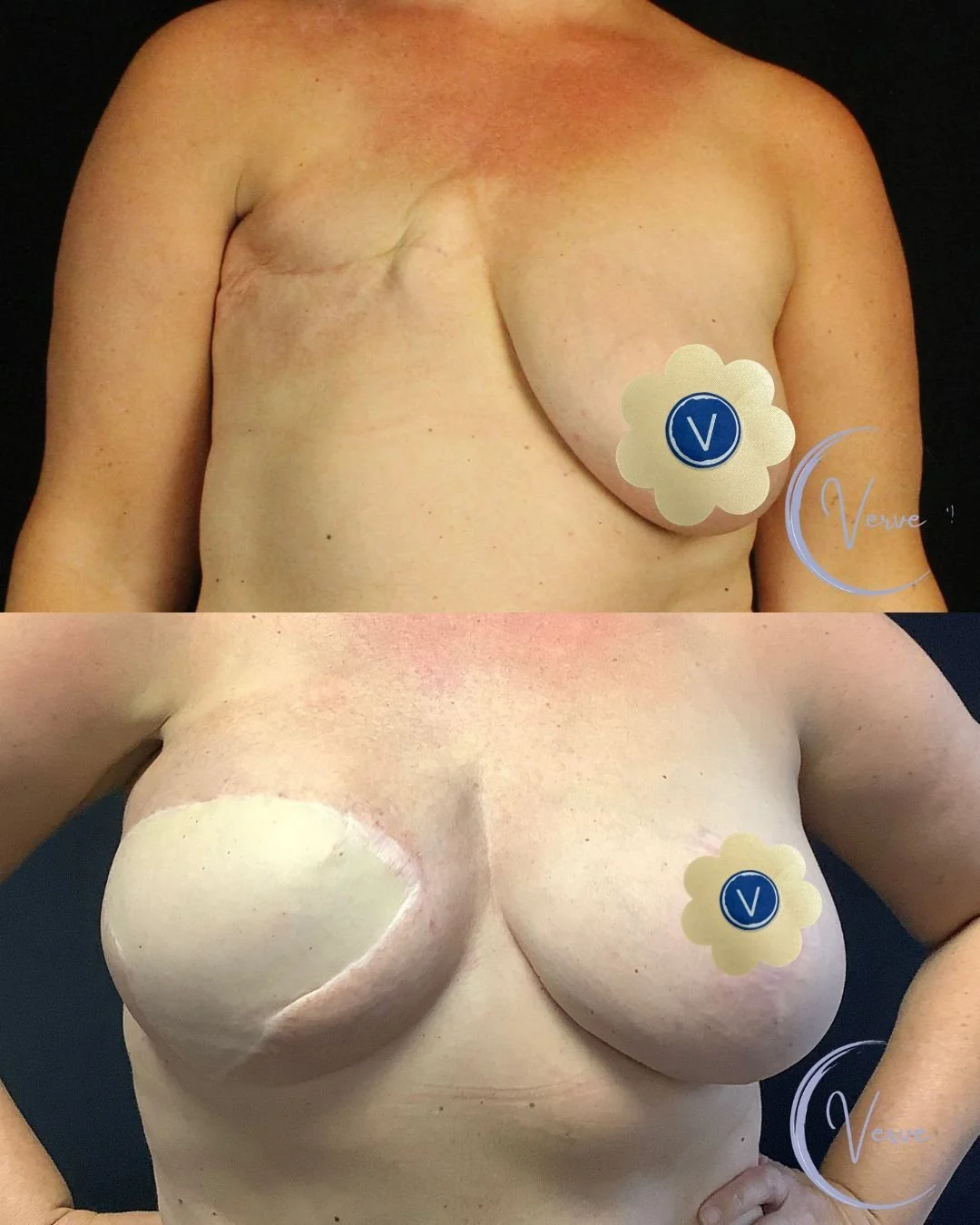
Latissimus and DIEP Flaps
Why get a Flap?
In some cases, implant-based reconstruction may not be the best option due to poor skin quality, radiation damage, multiple previous surgeries, or personal preference. When this happens, Dr. Gupta may recommend using your own tissue to rebuild the breast through a Latissimus Dorsi Flap (using skin, fat, and muscle from the back) or a DIEP Flap (using skin and fat from the lower abdomen).
These techniques can be an excellent solution for women who have thin or damaged skin, capsular contracture, or prefer to avoid implants altogether. Dr. Gupta will help you decide which flap is best suited to your body, lifestyle, and personal goals.
Latissimus Flap
-
The Latissimus Dorsi Flap is a type of breast reconstruction that uses muscle, skin, and fat from the upper back to help rebuild the breast after mastectomy or failed reconstruction. This tissue is tunneled under the skin to the chest to create a new breast shape, often combined with an implant for added volume.
-
This flap is often recommended for patients who have thin, damaged, or radiated skin that isn’t strong enough to hold an implant on its own. The flap provides healthy, well-vascularized tissue that improves healing, softens the breast, and reduces the risk of complications like capsular contracture.
-
In many cases, yes. The Latissimus Dorsi Flap provides coverage and support, but the volume of tissue from the back is usually not enough to match the desired breast size—so it’s often combined with a breast implant for fullness.
-
You will have a scar across the upper back, usually hidden beneath a bra or bathing suit line. Most women do not experience major changes in back strength or shoulder movement after healing.
-
Recovery usually takes a few weeks. You’ll need to limit lifting, reaching, and strenuous activity for several weeks while the tissues heal. Dr. Gupta and the Verve team will guide you through every step of the recovery process.
DIEP Flap
-
The DIEP Flap (Deep Inferior Epigastric Perforator Flap) is a type of breast reconstruction that uses skin and fat from the lower abdomen (similar to a tummy tuck) to rebuild the breast—without removing any muscle. This technique provides a soft, natural-looking breast using your own tissue.
-
A DIEP Flap is often recommended for women who:
Have had radiation therapy that damaged chest skin.
Prefer a natural option without implants.
Want a reconstruction that ages naturally and feels soft to the touch.
Have experienced implant complications or previous failed reconstruction.
Using your own tissue reduces the risk of long-term issues like implant rupture, capsular contracture, or visible rippling.
-
In most cases, no implant is needed. The DIEP Flap provides enough natural volume and shape on its own. Some women may choose to combine it with fat grafting or minor revisions later, but the goal is usually a fully autologous (your own tissue) reconstruction.
-
The tissue is taken from the lower belly, similar to the area treated in a tummy tuck. You’ll have a low horizontal scar (usually well-hidden by underwear or swimwear), and most women notice a flatter, tighter abdominal area after healing.
-
Recovery is longer than with implants—usually 4 to 6 weeks—because it involves healing both the chest and abdomen. You’ll need to avoid heavy lifting and strenuous activities for several weeks. Dr. Gupta and the Verve team will monitor you closely and provide detailed recovery instructions.
View the Gallery
Common Materials and Terms Used
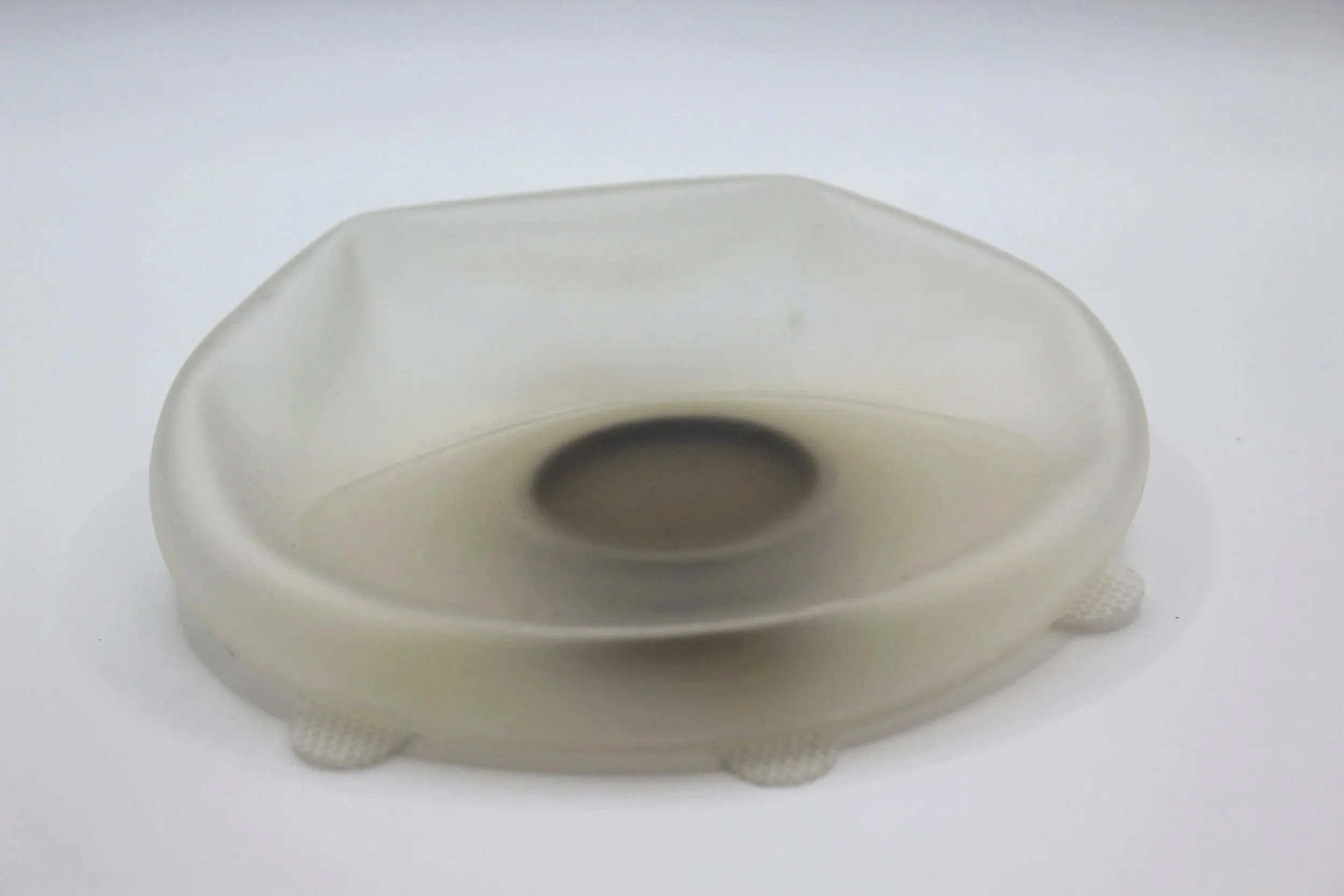
Tissue Expander
-
A tissue expander is often used for women who are undergoing a mastectomy and planning to have implant-based breast reconstruction. Since the skin and chest tissue are usually too tight or thin immediately after mastectomy, a tissue expander allows the area to be gradually stretched over time to safely accommodate a future breast implant.
-
A tissue expander is a temporary inflatable device placed under the chest muscle or skin. Over several weeks or months, small amounts of saline are added through a hidden valve, slowly stretching the skin and muscle to create space for the final implant.
-
During the expansion phase, the breast may look rounder, firmer, and less natural compared to the final result. The shape and softness will improve significantly once the expander is replaced with the permanent implant or combined with other reconstruction techniques.
-
Most patients describe the process as mildly uncomfortable with temporary tightness or pressure after each fill. Discomfort is typically brief and manageable with over-the-counter pain relief. Dr. Gupta and the Verve team will ensure your comfort throughout the process.
ActiShield™ Graft
-
The ActiShield™ graft is an amniotic-derived Acellular Dermal Matrix (ADM) used during breast reconstruction to provide internal support, promote healing, and help protect against bacterial contamination. Made from amniotic tissue, this biologic material is designed to support tissue regeneration and improve surgical outcomes in implant-based breast reconstruction.
-
Dr. Gupta may recommend using ActiShield™ if you are undergoing implant-based reconstruction after mastectomy, especially if your tissue is thin, weakened, or has been affected by radiation. The amniotic properties of the graft help to:
Support and stabilize the implant
Reduce inflammation and bacterial attachment
Encourage better healing and tissue strength
-
The ActiShield™ graft’s unique amniotic membrane properties naturally help resist bacterial adhesion, creating a healthier environment for both the implant and the healing tissue. This can lower the risk of infection and post-operative complications, particularly in higher-risk reconstruction cases.
-
Yes. The ActiShield™ graft gradually integrates with your natural tissue, becoming part of your body’s own structure. It provides lasting internal support and does not require removal.
ADM Graft
-
An ADM (Acellular Dermal Matrix) graft is a soft, biologic material made from processed human or animal tissue where all the cells have been removed. It is used in breast reconstruction to provide a protective layer over implants and to support proper healing by acting as a barrier to reduce the risk of infection and inflammation.
-
ADM grafts are often used in implant-based breast reconstruction—especially after mastectomy—to help lower the risk of complications such as infection, seroma (fluid buildup), or capsular contracture. They help create a healthier environment for the implant while your body heals and rebuilds.
-
The ADM graft itself does not change the outward look or shape of the breast. Its purpose is purely to support internal healing and protect the implant. Your final breast shape and softness come from the implant or tissue reconstruction, not the graft.
-
Yes. The ADM graft gradually integrates with your natural tissue, becoming part of your body over time. It is not removed and does not need to be replaced.
Check out the two brands of ADM we carry:
Stimulan® Beads
-
Stimulan® Beads are small, dissolvable beads made from calcium sulfate, designed to help prevent infection in surgical sites. They are often used in breast reconstruction or revision surgeries to deliver antibiotics directly to the area where an implant is placed, helping protect against post-operative infection.
-
Dr. Gupta may use Stimulan® Beads if you are at a higher risk for infection—such as in cases of breast revision, capsular contracture, or previous infection—or simply as an added layer of protection during your initial reconstruction. The beads help create a cleaner surgical environment by releasing high concentrations of antibiotics locally, exactly where they’re needed most.
-
After placement inside the surgical site, the Stimulan® Beads slowly dissolve over time, releasing antibiotics as they break down. This helps to reduce bacteria around the implant and can lower the risk of implant infection, biofilm formation, or complications that could require additional surgery.
-
No. Stimulan® Beads are fully dissolvable and are naturally absorbed by your body over a few weeks. They do not require removal and leave no permanent material behind.
Spy Imaging
-
SPY imaging is an advanced technology used during breast reconstruction surgery to help Dr. Gupta assess blood flow and tissue health in real time. It uses a special fluorescent dye and near-infrared light to visualize how well the tissue is receiving blood supply, which is crucial for successful healing.
-
SPY imaging helps ensure that the tissue used in your reconstruction is healthy and well-perfused. It’s especially useful in flap reconstructions (like DIEP or Latissimus) or when skin quality has been affected by radiation or previous surgeries. Additionally, in post-mastectomy reconstructions, SPY imaging is used to determine if there is enough blood flow in the skin to safely place a tissue expander. By identifying areas with poor blood flow, Dr. Gupta can make immediate adjustments to improve healing and reduce complications.
-
Yes. The imaging uses a safe, FDA-approved fluorescent dye called indocyanine green (ICG), which has been used in medicine for decades. The dye clears quickly from your body, and the procedure is non-invasive.
-
By showing tissue health during surgery, SPY imaging helps reduce the risk of tissue loss, improve cosmetic outcomes, and minimize the need for additional surgeries. This technology allows Dr. Gupta to provide the best possible long-term results.
Sign up for the Verve Standard Membership to access all pre-op and post-op instructions, recovery videos, and helpful tips and tricks—everything you need for the smoothest possible surgery experience.
Need to book an appointment?
info@verveplasticsurgery.com
(760) 436-7600
700 Garden View Ct STE 208
Encinitas, CA 92024